Prevention
| Exposure Route | Estimated infections per 10,000 exposures to an infected source | |||
|---|---|---|---|---|
| Blood Transfusion | 9,000[73] | |||
| Childbirth | 2,500[54] | |||
| Needle-sharing injection drug use | 67[74] | |||
| Percutaneous needle stick | 30[75] | |||
| Receptive anal intercourse* | 50[76][77] | |||
| Insertive anal intercourse* | 6.5[76][77] | |||
| Receptive penile-vaginal intercourse* | 10[76][77][78] | |||
| Insertive penile-vaginal intercourse* | 5[76][77] | |||
| Receptive oral intercourse*§ | 1[77] | |||
| Insertive oral intercourse*§ | 0.5[77] | |||
| * assuming no condom use § source refers to oral intercourse performed on a man | ||||
The three main transmission routes of HIV are sexual contact, exposure to infected body fluids or tissues, and from mother to fetus or child during perinatal period. It is possible to find HIV in the saliva, tears, and urine of infected individuals, but there are no recorded cases of infection by these secretions, and the risk of infection is negligible.[79]
Sexual contact
The majority of HIV infections are acquired through unprotected sexual relations between partners, one of whom has HIV. The primary mode of HIV infection worldwide is through sexual contact between members of the opposite sex.[80][81][82] During a sexual act, only male or female condoms can reduce the chances of infection with HIV and other STDs and the chances of becoming pregnant. The best evidence to date indicates that typical condom use reduces the risk of heterosexual HIV transmission by approximately 80% over the long-term, though the benefit is likely to be higher if condoms are used correctly on every occasion.[83] The male latex condom, if used correctly without oil-based lubricants, is the single most effective available technology to reduce the sexual transmission of HIV and other sexually transmitted infections. Manufacturers recommend that oil-based lubricants such as petroleum jelly, butter, and lard not be used with latex condoms, because they dissolve the latex, making the condoms porous. If necessary, manufacturers recommend using water-based lubricants. Oil-based lubricants can however be used with polyurethane condoms.[84]
The female condom is an alternative to the male condom and is made from polyurethane, which allows it to be used in the presence of oil-based lubricants. They are larger than male condoms and have a stiffened ring-shaped opening, and are designed to be inserted into the vagina. The female condom contains an inner ring, which keeps the condom in place inside the vagina – inserting the female condom requires squeezing this ring. However, at present availability of female condoms is very low and the price remains prohibitive for many women. Preliminary studies suggest that, where female condoms are available, overall protected sexual acts increase relative to unprotected sexual acts, making them an important HIV prevention strategy.[85]
Studies on couples where one partner is infected show that with consistent condom use, HIV infection rates for the uninfected partner are below 1% per year.[86] Prevention strategies are well-known in developed countries, however, recent epidemiological and behavioral studies in Europe and North America have suggested that a substantial minority of young people continue to engage in high-risk practices and that despite HIV/AIDS knowledge, young people underestimate their own risk of becoming infected with HIV.[87]
Randomized controlled trials have shown that male circumcision lowers the risk of HIV infection among heterosexual men by up to 60%.[88] It is expected that this procedure will be actively promoted in many of the countries affected by HIV, although doing so will involve confronting a number of practical, cultural and attitudinal issues. Some experts fear that a lower perception of vulnerability among circumcised men may result in more sexual risk-taking behavior, thus negating its preventive effects.[89]
Exposure to infected body fluids
Health care workers can reduce exposure to HIV by employing precautions to reduce the risk of exposure to contaminated blood. These precautions include barriers such as gloves, masks, protective eyeware or shields, and gowns or aprons which prevent exposure of the skin or mucous membranes to blood borne pathogens. Frequent and thorough washing of the skin immediately after being contaminated with blood or other bodily fluids can reduce the chance of infection. Finally, sharp objects like needles, scalpels and glass, are carefully disposed of to prevent needlestick injuries with contaminated items.[90] Since intravenous drug use is an important factor in HIV transmission in developed countries, harm reduction strategies such as needle-exchange programmes are used in attempts to reduce the infections caused by drug abuse.[91][92]
Mother-to-child transmission (MTCT)
Current recommendations state that when replacement feeding is acceptable, feasible, affordable, sustainable and safe, HIV-infected mothers should avoid breast-feeding their infant. However, if this is not the case, exclusive breast-feeding is recommended during the first months of life and discontinued as soon as possible.[93]
Treatment
- See also HIV Treatment and Antiretroviral drug.

There is currently no vaccine or cure for HIV or AIDS. The only known methods of prevention are based on avoiding exposure to the virus or, failing that, an antiretroviral treatment directly after a highly significant exposure, called post-exposure prophylaxis (PEP).[94] PEP has a very demanding four week schedule of dosage. It also has very unpleasant side effects including diarrhea, malaise, nausea and fatigue.[95]
Antiviral therapy
Current treatment for HIV infection consists of highly active antiretroviral therapy, or HAART.[96] This has been highly beneficial to many HIV-infected individuals since its introduction in 1996 when the protease inhibitor-based HAART initially became available.[9] Current optimal HAART options consist of combinations (or "cocktails") consisting of at least three drugs belonging to at least two types, or "classes," of antiretroviral agents. Typical regimens consist of two nucleoside analogue reverse transcriptase inhibitors (NARTIs or NRTIs) plus either a protease inhibitor or a non-nucleoside reverse transcriptase inhibitor (NNRTI). Because HIV disease progression in children is more rapid than in adults, and laboratory parameters are less predictive of risk for disease progression, particularly for young infants, treatment recommendations are more aggressive for children than for adults.[97] In developed countries where HAART is available, doctors assess the viral load, rapidity in CD4 decline, and patient readiness while deciding when to recommend initiating treatment.[98]
HAART allows the stabilization of the patient’s symptoms and viremia, but it neither cures the patient of HIV, nor alleviates the symptoms, and high levels of HIV-1, often HAART resistant, return once treatment is stopped.[99][100] Moreover, it would take more than the lifetime of an individual to be cleared of HIV infection using HAART.[101] Despite this, many HIV-infected individuals have experienced remarkable improvements in their general health and quality of life, which has led to the plummeting of HIV-associated morbidity and mortality.[102][103][104] In the absence of HAART, progression from HIV infection to AIDS occurs at a median of between nine to ten years and the median survival time after developing AIDS is only 9.2 months.[31] HAART is thought to increase survival time by between 4 and 12 years.[105][106]
For some patients, which can be more than fifty percent of patients, HAART achieves far less than optimal results, due to medication intolerance/side effects, prior ineffective antiretroviral therapy and infection with a drug-resistant strain of HIV. Non-adherence and non-persistence with therapy are the major reasons why some people do not benefit from HAART.[107] The reasons for non-adherence and non-persistence are varied. Major psychosocial issues include poor access to medical care, inadequate social supports, psychiatric disease and drug abuse. HAART regimens can also be complex and thus hard to follow, with large numbers of pills taken frequently.[108][109][110] Side effects can also deter people from persisting with HAART, these include lipodystrophy, dyslipidaemia, diarrhoea, insulin resistance, an increase in cardiovascular risks and birth defects.[111] Anti-retroviral drugs are expensive, and the majority of the world's infected individuals do not have access to medications and treatments for HIV and AIDS.
Future research
It has been postulated that only a vaccine can halt the pandemic because a vaccine would possibly cost less, thus being affordable for developing countries, and would not require daily treatments. However, even after almost 30 years of research, HIV-1 remains a difficult target for a vaccine.[112]
Research to improve current treatments includes decreasing side effects of current drugs, further simplifying drug regimens to improve adherence, and determining the best sequence of regimens to manage drug resistance. A number of studies have shown that measures to prevent opportunistic infections can be beneficial when treating patients with HIV infection or AIDS. Vaccination against hepatitis A and B is advised for patients who are not infected with these viruses and are at risk of becoming infected.[113] Patients with substantial immunosuppression are also advised to receive prophylactic therapy for Pneumocystis jiroveci pneumonia (PCP), and many patients may benefit from prophylactic therapy for toxoplasmosis and Cryptococcus meningitis as well.[95]
Researchers have discovered an abzyme that can destroy the protein gp120 CD4 binding site. This protein is common to all HIV variants as it is the attachment point for B lymphocytes and subsequent compromising of the immune system.[114]
Alternative medicine
Various forms of alternative medicine have been used to treat symptoms or alter the course of the disease.[115] Acupuncture has been used to alleviate some symptoms, such peripheral neuropathy, but cannot cure the HIV infection.[116] Several randomized clinical trials testing the effect of herbal medicines have shown that there is no evidence that these herbs have any effect on the progression of the disease, but may instead produce serious side-effects.[117]
Some data suggest that multivitamin and mineral supplements might reduce HIV disease progression in adults, although there is no conclusive evidence on if they reduce mortality among people with good nutritional status.[118] Vitamin A supplementation in children probably has some benefit.[118] Daily doses of selenium can suppress HIV viral burden with an associated improvement of the CD4 count. Selenium can be used as an adjunct therapy to standard antiviral treatments, but cannot itself reduce mortality and morbidity.[119]
Current studies indicate that that alternative medicine therapies have little effect on the mortality or morbidity of the disease, but may improve the quality of life of individuals afflicted with AIDS. The psychological benefits of these therapies are the most important use.[115]
Prognosis
Without treatment, the net median survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype,[5] and the median survival rate after diagnosis of AIDS in resource-limited settings where treatment is not available ranges between 6 and 19 months, depending on the study.[120] In areas where it is widely available, the development of HAART as effective therapy for HIV infection and AIDS reduced the death rate from this disease by 80%, and raised the life expectancy for a newly-diagnosed HIV-infected person to about 20 years.[121]
As new treatments continue to be developed and because HIV continues to evolve resistance to treatments, estimates of survival time are likely to continue to change. Without antiretroviral therapy, death normally occurs within a year.[31] Most patients die from opportunistic infections or malignancies associated with the progressive failure of the immune system.[122] The rate of clinical disease progression varies widely between individuals and has been shown to be affected by many factors such as host susceptibility and immune function[32][33][36] health care and co-infections,[31][122] as well as which particular strain of the virus is involved.[38][123][124]
Epidemiology
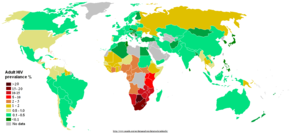
The AIDS pandemic can also be seen as several epidemics of separate subtypes; the major factors in its spread are sexual transmission and vertical transmission from mother to child at birth and through breast milk.[4] Despite recent, improved access to antiretroviral treatment and care in many regions of the world, the AIDS pandemic claimed an estimated 2.1 million (range 1.9–2.4 million) lives in 2007 of which an estimated 330,000 were children under 15 years.[5] Globally, an estimated 33.2 million people lived with HIV in 2007, including 2.5 million children. An estimated 2.5 million (range 1.8–4.1 million) people were newly infected in 2007, including 420,000 children.[5]
Sub-Saharan Africa remains by far the worst affected region. In 2007 it contained an estimated 68% of all people living with AIDS and 76% of all AIDS deaths, with 1.7 million new infections bringing the number of people living with HIV to 22.5 million, and with 11.4 million AIDS orphans living in the region. Unlike other regions, most people living with HIV in sub-Saharan Africa in 2007 (61%) were women. Adult prevalence in 2007 was an estimated 5.0%, and AIDS continued to be the single largest cause of mortality in this region.[5] South Africa has the largest population of HIV patients in the world, followed by Nigeria and India.[125] South & South East Asia are second worst affected; in 2007 this region contained an estimated 18% of all people living with AIDS, and an estimated 300,000 deaths from AIDS.[5] India has an estimated 2.5 million infections and an estimated adult prevalence of 0.36%.[5] Life expectancy has fallen dramatically in the worst-affected countries; for example, in 2006 it was estimated that it had dropped from 65 to 35 years in Botswana.[4]
History
AIDS was first reported June 5, 1981, when the U.S. Centers for Disease Control and Prevention recorded a cluster of Pneumocystis carinii pneumonia (now still classified as PCP but known to be caused by Pneumocystis jirovecii) in five homosexual men in Los Angeles.[126] In the beginning, the Centers for Disease Control and Prevention (CDC) did not have an official name for the disease, often referring to it by way of the diseases that were associated with it, for example, lymphadenopathy, the disease after which the discoverers of HIV originally named the virus.[66][67] They also used Kaposi's Sarcoma and Opportunistic Infections, the name by which a task force had been set up in 1981.[127] In the general press, the term GRID, which stood for Gay-related immune deficiency, had been coined.[128] The CDC, in search of a name, and looking at the infected communities coined “the 4H disease,” as it seemed to single out Haitians, homosexuals, hemophiliacs, and heroin users.[129] However, after determining that AIDS was not isolated to the homosexual community,[127] the term GRID became misleading and AIDS was introduced at a meeting in July 1982.[130] By September 1982 the CDC started using the name AIDS, and properly defined the illness.[131]
A more controversial theory known as the OPV AIDS hypothesis suggests that the AIDS epidemic was inadvertently started in the late 1950s in the Belgian Congo by Hilary Koprowski's research into a poliomyelitis vaccine.[132][133] According to scientific consensus, this scenario is not supported by the available evidence.[134][135][136]
A recent study states that HIV probably moved from Africa to Haiti and then entered the United States around 1969.[137]
Also see AIDS origins opposed to scientific consensus
Society and culture
Stigma

AIDS stigma exists around the world in a variety of ways, including ostracism, rejection, discrimination and avoidance of HIV infected people; compulsory HIV testing without prior consent or protection of confidentiality; violence against HIV infected individuals or people who are perceived to be infected with HIV; and the quarantine of HIV infected individuals.[138] Stigma-related violence or the fear of violence prevents many people from seeking HIV testing, returning for their results, or securing treatment, possibly turning what could be a manageable chronic illness into a death sentence and perpetuating the spread of HIV.[139]
AIDS stigma has been further divided into the following three categories:
- Instrumental AIDS stigma—a reflection of the fear and apprehension that are likely to be associated with any deadly and transmissible illness.[140]
- Symbolic AIDS stigma—the use of HIV/AIDS to express attitudes toward the social groups or lifestyles perceived to be associated with the disease.[140]
- Courtesy AIDS stigma—stigmatization of people connected to the issue of HIV/AIDS or HIV- positive people.[141]
Often, AIDS stigma is expressed in conjunction with one or more other stigmas, particularly those associated with homosexuality, bisexuality, promiscuity, and intravenous drug use.
In many developed countries, there is an association between AIDS and homosexuality or bisexuality, and this association is correlated with higher levels of sexual prejudice such as anti-homosexual attitudes.[142] There is also a perceived association between AIDS and all male-male sexual behavior, including sex between uninfected men.[140]
Economic impact
HIV and AIDS affects economic growth by reducing the availability of human capital.[6] Without proper nutrition, health care and medicine that is available in developed countries, large numbers of people are falling victim to AIDS. They will not only be unable to work, but will also require significant medical care. The forecast is that this will likely cause a collapse of economies and societies in countries with a significant AIDS populationi. In some heavily infected areas, the epidemic has left behind many orphans cared for by elderly grandparents.[143]
The increased mortality in this region will result in a smaller skilled population and labor force. This smaller labor force will be predominantly young people, with reduced knowledge and work experience leading to reduced productivity. An increase in workers’ time off to look after sick family members or for sick leave will also lower productivity. Increased mortality will also weaken the mechanisms that generate human capital and investment in people, through loss of income and the death of parents. By killing off mainly young adults, AIDS seriously weakens the taxable population, reducing the resources available for public expenditures such as education and health services not related to AIDS resulting in increasing pressure for the state's finances and slower growth of the economy. This results in a slower growth of the tax base, an effect that will be reinforced if there are growing expenditures on treating the sick, training (to replace sick workers), sick pay and caring for AIDS orphans. This is especially true if the sharp increase in adult mortality shifts the responsibility and blame from the family to the government in caring for these orphans.[143]
On the level of the household, AIDS results in both the loss of income and increased spending on healthcare by the household. The income effects of this lead to spending reduction as well as a substitution effect away from education and towards healthcare and funeral spending. A study in Côte d'Ivoire showed that households with an HIV/AIDS patient spent twice as much on medical expenses as other households.[144]
AIDS denialism
A small group of activists, including several scientists who do not study HIV/AIDS, question the connection between HIV and AIDS,[145] the existence of HIV itself,[146] or the validity of current testing and treatment methods. Though these claims have been examined and thoroughly rejected by the scientific community,[147] they continue to be promulgated through the Internet[148] and have had a significant political impact, particularly in South Africa, where President Thabo Mbeki's embrace of AIDS denialism has been blamed for an ineffective response to that country's AIDS epidemic.[149][150][151]
Notes and references
- ^ Weiss RA (May 1993). "How does HIV cause AIDS?". Science (journal) 260 (5112): 1273–9. PMID 8493571.
- ^ Divisions of HIV/AIDS Prevention (2003). "HIV and Its Transmission". Centers for Disease Control & Prevention. Retrieved on 2006-05-23.
- ^ San Francisco AIDS Foundation (2006-04-14). "How HIV is spread". Retrieved on 2006-05-23.
- ^ a b c Kallings LO (2008). "The first postmodern pandemic: 25 years of HIV/AIDS". J Intern Med 263 (3): 218–43. doi:. PMID 18205765.
- ^ a b c d e f g h UNAIDS, WHO (December 2007). "2007 AIDS epidemic update" (PDF). Retrieved on 2008-03-12.
- ^ a b Bell C, Devarajan S, Gersbach H. "The long-run economic costs of AIDS: theory and an application to South Africa" (PDF). World Bank Policy Research Working Paper No. 3152. Retrieved on 2008-04-28.
- ^ Gao F, Bailes E, Robertson DL, et al (1999). "Origin of HIV-1 in the Chimpanzee Pan troglodytes troglodytes". Nature 397 (6718): 436–441. doi:. PMID 9989410.
- ^ Gallo RC (2006). "A reflection on HIV/AIDS research after 25 years". Retrovirology 3: 72. doi:. PMID 17054781.
- ^ a b Palella FJ Jr, Delaney KM, Moorman AC, et al (1998). "Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators". N. Engl. J. Med 338 (13): 853–860. PMID 9516219.
- ^ Holmes CB, Losina E, Walensky RP, Yazdanpanah Y, Freedberg KA (2003). "Review of human immunodeficiency virus type 1-related opportunistic infections in sub-Saharan Africa". Clin. Infect. Dis. 36 (5): 656–662. PMID 12594648.
- ^ Guss DA (1994). "The acquired immune deficiency syndrome: an overview for the emergency physician, Part 1". J. Emerg. Med. 12 (3): 375–384. PMID 8040596.
- ^ Guss DA (1994). "The acquired immune deficiency syndrome: an overview for the emergency physician, Part 2". J. Emerg. Med. 12 (4): 491–497. PMID 7963396.
- ^ Feldman C (2005). "Pneumonia associated with HIV infection". Curr. Opin. Infect. Dis. 18 (2): 165–170. PMID 15735422.
- ^ Decker CF, Lazarus A (2000). "Tuberculosis and HIV infection. How to safely treat both disorders concurrently". Postgrad Med. 108 (2): 57–60, 65–68. PMID 10951746.
- ^ Zaidi SA, Cervia JS (2002). "Diagnosis and management of infectious esophagitis associated with human immunodeficiency virus infection". J. Int. Assoc. Physicians AIDS Care (Chic Ill) 1 (2): 53–62. PMID 12942677.
- ^ Pollok RC (2001). "Viruses causing diarrhoea in AIDS". Novartis Found. Symp. 238: 276–83; discussion 283–8. PMID 11444032.
- ^ Guerrant RL, Hughes JM, Lima NL, Crane J (1990). "Diarrhea in developed and developing countries: magnitude, special settings, and etiologies". Rev. Infect. Dis. 12 (Suppl 1): S41–S50. PMID 2406855.
- ^ Luft BJ, Chua A (2000). "Central Nervous System Toxoplasmosis in HIV Pathogenesis, Diagnosis, and Therapy". Curr. Infect. Dis. Rep. 2 (4): 358–362. PMID 11095878.
- ^ Sadler M, Nelson MR (1997). "Progressive multifocal leukoencephalopathy in HIV". Int. J. STD AIDS 8 (6): 351–357. PMID 9179644.
- ^ Gray F, Adle-Biassette H, Chrétien F, Lorin de la Grandmaison G, Force G, Keohane C (2001). "Neuropathology and neurodegeneration in human immunodeficiency virus infection. Pathogenesis of HIV-induced lesions of the brain, correlations with HIV-associated disorders and modifications according to treatments". Clin. Neuropathol. 20 (4): 146–155. PMID 11495003.
- ^ Grant I, Sacktor H, McArthur J (2005). "HIV neurocognitive disorders", in H. E. Gendelman, I. Grant, I. Everall, S. A. Lipton, and S. Swindells. (ed.): The Neurology of AIDS (PDF), 2nd, London, UK: Oxford University Press, 357–373. ISBN 0-19-852610-5.
- ^ Satishchandra P, Nalini A, Gourie-Devi M, et al (2000). "Profile of neurologic disorders associated with HIV/AIDS from Bangalore, South India (1989–1996)". Indian J. Med. Res. 11: 14–23. PMID 10793489.
- ^ Wadia RS, Pujari SN, Kothari S, Udhar M, Kulkarni S, Bhagat S, Nanivadekar A (2001). "Neurological manifestations of HIV disease". J. Assoc. Physicians India 49: 343–348. PMID 11291974.
- ^ Boshoff C, Weiss R (2002). "AIDS-related malignancies". Nat. Rev. Cancer 2 (5): 373–382. PMID 12044013.
- ^ Yarchoan R, Tosatom G, Littlem RF (2005). "Therapy insight: AIDS-related malignancies — the influence of antiviral therapy on pathogenesis and management". Nat. Clin. Pract. Oncol. 2 (8): 406–415. PMID 16130937.
- ^ Palefsky J (2007). "Human papillomavirus infection in HIV-infected persons". Top HIV Med 15 (4): 130–3. PMID 17720998.
- ^ Bonnet F, Lewden C, May T, et al (2004). "Malignancy-related causes of death in human immunodeficiency virus-infected patients in the era of highly active antiretroviral therapy". Cancer 101 (2): 317–324. PMID 15241829.
- ^ Skoulidis F, Morgan MS, MacLeod KM (2004). "Penicillium marneffei: a pathogen on our doorstep?". J. R. Soc. Med. 97 (2): 394–396. PMID 15286196.
- ^ Alimonti JB, Ball TB, Fowke KR (2003). "Mechanisms of CD4+ T lymphocyte cell death in human immunodeficiency virus infection and AIDS.". J. Gen. Virol. 84 (7): 1649–1661. doi:. PMID 12810858.
- ^ (2003) An Atlas of Differential Diagnosis in HIV Disease, Second Edition. CRC Press-Parthenon Publishers, 22-27. ISBN 1-84214-026-4.
- ^ a b c d e Morgan D, Mahe C, Mayanja B, Okongo JM, Lubega R, Whitworth JA (2002). "HIV-1 infection in rural Africa: is there a difference in median time to AIDS and survival compared with that in industrialized countries?". AIDS 16 (4): 597–632. PMID 11873003.
- ^ a b Clerici M, Balotta C, Meroni L, et al (1996). "Type 1 cytokine production and low prevalence of viral isolation correlate with long-term non progression in HIV infection". AIDS Res. Hum. Retroviruses. 12 (11): 1053–1061. PMID 8827221.
- ^ a b Morgan D, Mahe C, Mayanja B, Whitworth JA (2002). "Progression to symptomatic disease in people infected with HIV-1 in rural Uganda: prospective cohort study". BMJ 324 (7331): 193–196. doi:. PMID 11809639.
- ^ Gendelman HE, Phelps W, Feigenbaum L, et al (1986). "Transactivation of the human immunodeficiency virus long terminal repeat sequences by DNA viruses". Proc. Natl. Acad. Sci. U. S. A. 83 (24): 9759–9763. PMID 2432602.
- ^ Bentwich Z, Kalinkovich, A, Weisman Z (1995). "Immune activation is a dominant factor in the pathogenesis of African AIDS.". Immunol. Today 16 (4): 187–191. PMID 7734046.
- ^ a b Tang J, Kaslow RA (2003). "The impact of host genetics on HIV infection and disease progression in the era of highly active antiretroviral therapy". AIDS 17 (Suppl 4): S51–S60. PMID 15080180.
- ^ Quiñones-Mateu ME, Mas A, Lain de Lera T, Soriano V, Alcami J, Lederman MM, Domingo E (1998). "LTR and tat variability of HIV-1 isolates from patients with divergent rates of disease progression". Virus Research 57 (1): 11–20. PMID 9833881.
- ^ a b Campbell GR, Pasquier E, Watkins J, et al (2004). "The glutamine-rich region of the HIV-1 Tat protein is involved in T-cell apoptosis". J. Biol. Chem. 279 (46): 48197–48204. doi:. PMID 15331610.
- ^ Kaleebu P, French N, Mahe C, et al (2002). "Effect of human immunodeficiency virus (HIV) type 1 envelope subtypes A and D on disease progression in a large cohort of HIV-1-positive persons in Uganda". J. Infect. Dis. 185 (9): 1244–1250. PMID 12001041.
- ^ Rothenberg RB, Scarlett M, del Rio C, Reznik D, O'Daniels C (1998). "Oral transmission of HIV". AIDS 12 (16): 2095–2105. PMID 9833850.
- ^ Mastro TD, de Vincenzi I (1996). "Probabilities of sexual HIV-1 transmission". AIDS 10 (Suppl A): S75–S82. PMID 8883613.
- ^ Koenig MA, Zablotska I, Lutalo T, Nalugoda F, Wagman J, Gray R (2004). "Coerced first intercourse and reproductive health among adolescent women in Rakai, Uganda". Int Fam Plan Perspect 30 (4): 156–63. doi:. PMID 15590381.
- ^ a b Laga M, Nzila N, Goeman J (1991). "The interrelationship of sexually transmitted diseases and HIV infection: implications for the control of both epidemics in Africa". AIDS 5 (Suppl 1): S55–S63. PMID 1669925.
- ^ Tovanabutra S, Robison V, Wongtrakul J, et al (2002). "Male viral load and heterosexual transmission of HIV-1 subtype E in northern Thailand". J. Acquir. Immune. Defic. Syndr. 29 (3): 275–283. PMID 11873077.
- ^ Sagar M, Lavreys L, Baeten JM, et al (2004). "Identification of modifiable factors that affect the genetic diversity of the transmitted HIV-1 population". AIDS 18 (4): 615–619. PMID 15090766.
- ^ Lavreys L, Baeten JM, Martin HL, et al (March 2004). "Hormonal contraception and risk of HIV-1 acquisition: results of a 10-year prospective study". AIDS 18 (4): 695–7. PMID 15090778.
- ^ Epstein, Helen (2007). The invisible cure: Africa, the West, and the fight against AIDS. New York: Farrar, Straus, and Giroux. ISBN 0-374-28152-1.
- ^ Parasitic worms may boost African HIV rates
- ^ Agnès-Laurence Chenine, Ela Shai-Kobiler, Lisa N. Steele, Helena Ong, Peter Augostini, Ruijiang Song, Sandra J. Lee, Patrick Autissier, Ruth M. Ruprecht, W. Evan Secor Acute Schistosoma mansoni Infection Increases Susceptibility to Systemic SHIV Clade C Infection in Rhesus Macaques after Mucosal Virus Exposure PLoS Neglected Tropical Diseases DOI: 10.1371/journal.pntd.0000265
- ^ Fan H (2005). in Fan, H., Conner, R. F. and Villarreal, L. P. eds: AIDS: science and society, 4th, Boston, MA: Jones and Bartlett Publishers. ISBN 0-7637-0086-X.
- ^ "WHO, UNAIDS Reaffirm HIV as a Sexually Transmitted Disease". WHO (2003-03-17). Retrieved on 2006-01-17.
- ^ "Financial Resources Required to Achieve, Universal Access to HIV Prevention, Treatment Care and Support" (pdf). UNAIDS. Retrieved on 2008-04-11.
- ^ "Blood safety....for too few". WHO (2001). Retrieved on 2006-01-17.
- ^ a b Coovadia H (2004). "Antiretroviral agents—how best to protect infants from HIV and save their mothers from AIDS". N. Engl. J. Med. 351 (3): 289–292. PMID 15247337.
- ^ Coovadia HM, Bland RM (2007). "Preserving breastfeeding practice through the HIV pandemic". Trop. Med. Int. Health. 12 (9): 1116–1133. PMID 17714431.
- ^ Blechner MJ (1997). Hope and mortality: psychodynamic approaches to AIDS and HIV. Hillsdale, NJ: Analytic Press. ISBN 0-88163-223-6.
- ^ Guss DA (1994). "The acquired immune deficiency syndrome: an overview for the emergency physician, Part 1". J Emerg Med 12 (3): 375–84. PMID 8040596.
- ^ Hel Z, McGhee JR, Mestecky J (June 2006). "HIV infection: first battle decides the war". Trends Immunol. 27 (6): 274–81. doi:. PMID 16679064.
- ^ Mehandru S, Poles MA, Tenner-Racz K, Horowitz A, Hurley A, Hogan C, Boden D, Racz P, Markowitz M (September 2004). "Primary HIV-1 infection is associated with preferential depletion of CD4+ T lymphocytes from effector sites in the gastrointestinal tract". J. Exp. Med. 200 (6): 761–70. doi:. PMID 15365095.
- ^ Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, Nguyen PL, Khoruts A, Larson M, Haase AT, Douek DC (September 2004). "CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract". J. Exp. Med. 200 (6): 749–59. doi:. PMID 15365096.
- ^ Appay V, Sauce D (January 2008). "Immune activation and inflammation in HIV-1 infection: causes and consequences". J. Pathol. 214 (2): 231–41. doi:. PMID 18161758.
- ^ Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, Kazzaz Z, Bornstein E, Lambotte O, Altmann D, Blazar BR, Rodriguez B, Teixeira-Johnson L, Landay A, Martin JN, Hecht FM, Picker LJ, Lederman MM, Deeks SG, Douek DC (December 2006). "Microbial translocation is a cause of systemic immune activation in chronic HIV infection". Nat. Med. 12 (12): 1365–71. doi:. PMID 17115046.
- ^ Textbook of Pathology by Harsh Mohan, ISBN 81-8061-368-2
- ^ Textbook of Pathology by Harsh Mohan, ISBN 81-8061-368-2
- ^ World Health Organization (1990). "Interim proposal for a WHO staging system for HIV infection and disease". WHO Wkly Epidem. Rec. 65 (29): 221–228. PMID 1974812.
- ^ a b Centers for Disease Control (CDC) (1982). "Persistent, generalized lymphadenopathy among homosexual males.". MMWR Morb Mortal Wkly Rep. 31 (19): 249–251. PMID 6808340.
- ^ a b Barré-Sinoussi F, Chermann JC, Rey F, et al (1983). "Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS)". Science 220 (4599): 868–871. doi:. PMID 6189183.
- ^ "1993 Revised Classification System for HIV Infection and Expanded Surveillance Case Definition for AIDS Among Adolescents and Adults". CDC (1992). Retrieved on 2006-02-09.
- ^ a b Kumaranayake L, Watts C (2001). "Resource allocation and priority setting of HIV/AIDS interventions: addressing the generalized epidemic in sub-Saharan Africa". J. Int. Dev. 13 (4): 451–466. doi:.
- ^ Weber B (2006). "Screening of HIV infection: role of molecular and immunological assays". Expert Rev. Mol. Diagn. 6 (3): 399–411. doi:. PMID 16706742.
- ^ Tóth FD, Bácsi A, Beck Z, Szabó J (2001). "Vertical transmission of human immunodeficiency virus". Acta Microbiol Immunol Hung 48 (3-4): 413–27. doi:. PMID 11791341.
- ^ Smith DK, Grohskopf LA, Black RJ, et al (2005). "Antiretroviral Postexposure Prophylaxis After Sexual, Injection-Drug Use, or Other Nonoccupational Exposure to HIV in the United States". MMWR 54 (RR02): 1–20.
- ^ Donegan E, Stuart M, Niland JC, et al (1990). "Infection with human immunodeficiency virus type 1 (HIV-1) among recipients of antibody-positive blood donations". Ann. Intern. Med. 113 (10): 733–739. PMID 2240875.
- ^ Kaplan EH, Heimer R (1995). "HIV incidence among New Haven needle exchange participants: updated estimates from syringe tracking and testing data". J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 10 (2): 175–176. PMID 7552482.
- ^ Bell DM (1997). "Occupational risk of human immunodeficiency virus infection in healthcare workers: an overview.". Am. J. Med. 102 (5B): 9–15. PMID 9845490.
- ^ a b c d European Study Group on Heterosexual Transmission of HIV (1992). "Comparison of female to male and male to female transmission of HIV in 563 stable couples". BMJ. 304 (6830): 809–813. PMID 1392708.
- ^ a b c d e f Varghese B, Maher JE, Peterman TA, Branson BM,Steketee RW (2002). "Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use". Sex. Transm. Dis. 29 (1): 38–43. PMID 11773877.
- ^ Leynaert B, Downs AM, de Vincenzi I (1998). "Heterosexual transmission of human immunodeficiency virus: variability of infectivity throughout the course of infection. European Study Group on Heterosexual Transmission of HIV". Am. J. Epidemiol. 148 (1): 88–96. PMID 9663408.
- ^ "Facts about AIDS & HIV". avert.org. Retrieved on 2007-11-30.
- ^ Johnson AM, Laga M (1988). "Heterosexual transmission of HIV". AIDS 2 (suppl. 1): S49-S56. PMID 3130121.
- ^ N'Galy B, Ryder RW (1988). "Epidemiology of HIV infection in Africa". Journal of Acquired Immune Deficiency Syndromes 1 (6): 551-558. PMID 3225742.
- ^ Deschamps MM, Pape JW, Hafner A, Johnson WD Jr. (1996). "Heterosexual transmission of HIV in Haiti". Annals of Internal Medicine 125 (4): 324–330. PMID 8678397.
- ^ Cayley WE Jr. (2004). "Effectiveness of condoms in reducing heterosexual transmission of HIV". Am. Fam. Physician 70 (7): 1268–1269. PMID 15508535.
- ^ "Module 5/Guidelines for Educators" (Microsoft Word). Durex. Retrieved on 2006-04-17.
- ^ PATH (2006). "The female condom: significant potential for STI and pregnancy prevention". Outlook 22 (2).
- ^ "Condom Facts and Figures". WHO (August 2003). Retrieved on 2006-01-17.
- ^ Dias SF, Matos MG, Goncalves, A. C. (2005). "Preventing HIV transmission in adolescents: an analysis of the Portuguese data from the Health Behaviour School-aged Children study and focus groups". Eur. J. Public Health 15 (3): 300–304. PMID 15941747.
- ^ Weiss HA (February 2007). "Male circumcision as a preventive measure against HIV and other sexually transmitted diseases". Curr. Opin. Infect. Dis. 20 (1): 66–72. doi:. PMID 17197884.
- ^ Eaton LA, Kalichman S (December 2007). "Risk compensation in HIV prevention: implications for vaccines, microbicides, and other biomedical HIV prevention technologies". Curr HIV/AIDS Rep 4 (4): 165–72. doi:. PMID 18366947.
- ^ "Recommendations for Prevention of HIV Transmission in Health-Care Settings". Retrieved on 2008-04-28.
- ^ Kerr T, Kimber J, Debeck K, Wood E (December 2007). "The role of safer injection facilities in the response to HIV/AIDS among injection drug users". Curr HIV/AIDS Rep 4 (4): 158–64. doi:. PMID 18366946.
- ^ Wodak A, Cooney A (2006). "Do needle syringe programs reduce HIV infection among injecting drug users: a comprehensive review of the international evidence". Subst Use Misuse 41 (6-7): 777–813. doi:. PMID 16809167.
- ^ WHO HIV and Infant Feeding Technical Consultation (2006). "Consensus statement" (PDF). Retrieved on 2008-03-12.
- ^ Hamlyn E, Easterbrook P (August 2007). "Occupational exposure to HIV and the use of post-exposure prophylaxis". Occup Med (Lond) 57 (5): 329–36. doi:. PMID 17656498.
- ^ a b "A Pocket Guide to Adult HIV/AIDS Treatment February 2006 edition". Department of Health and Human Services (February 2006). Retrieved on 2006-09-01.
- ^ "A Pocket Guide to Adult HIV/AIDS Treatment February 2006 edition". Department of Health and Human Services (February 2006). Retrieved on 2006-09-01.
- ^ "Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection" (PDF). Department of Health and Human Services Working Group on Antiretroviral Therapy and Medical Management of HIV-Infected Children (2005-11-03). Retrieved on 2006-01-17.
- ^ "Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents" (PDF). Department of Health and Human Services Panel on Clinical Practices for Treatment of HIV Infection (2005-10-06). Retrieved on 2006-01-17.
- ^ Martinez-Picado J, DePasquale MP, Kartsonis N, et al (2000). "Antiretroviral resistance during successful therapy of human immunodeficiency virus type 1 infection". Proc. Natl. Acad. Sci. U. S. A. 97 (20): 10948–10953. PMID 11005867.
- ^ Dybul M, Fauci AS, Bartlett JG, Kaplan JE, Pau AK; Panel on Clinical Practices for Treatment of HIV. (2002). "Guidelines for using antiretroviral agents among HIV-infected adults and adolescents". Ann. Intern. Med. 137 (5 Pt 2): 381–433. PMID 12617573.
- ^ Blankson JN, Persaud D, Siliciano RF (2002). "The challenge of viral reservoirs in HIV-1 infection". Annu. Rev. Med. 53: 557–593. PMID 11818490.
- ^ Palella FJ, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Aschman DJ, Holmberg SD (1998). "Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection". N. Engl. J. Med. 338 (13): 853–860. PMID 9516219.
- ^ Wood E, Hogg RS, Yip B, Harrigan PR, O'Shaughnessy MV, Montaner JS (2003). "Is there a baseline CD4 cell count that precludes a survival response to modern antiretroviral therapy?". AIDS 17 (5): 711–720. PMID 12646794.
- ^ Chene G, Sterne JA, May M, Costagliola D, Ledergerber B, Phillips AN, Dabis F, Lundgren J, D'Arminio Monforte A, de Wolf F, Hogg R, Reiss P, Justice A, Leport C, Staszewski S, Gill J, Fatkenheuer G, Egger ME and the Antiretroviral Therapy Cohort Collaboration (2003). "Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies". Lancet 362 (9385): 679–686. doi:. PMID 12957089.
- ^ King JT, Justice AC, Roberts MS, Chang CH, Fusco JS and the CHORUS Program Team (2003). "Long-Term HIV/AIDS Survival Estimation in the Highly Active Antiretroviral Therapy Era". Medical Decision Making 23 (1): 9–20. PMID 12583451.
- ^ Tassie JM, Grabar S, Lancar R, Deloumeaux J, Bentata M, Costagliola D and the Clinical Epidemiology Group from the French Hospital Database on HIV (2002). "Time to AIDS from 1992 to 1999 in HIV-1-infected subjects with known date of infection". Journal of acquired immune deficiency syndromes 30 (1): 81–7. PMID 12048367.
- ^ Becker SL, Dezii CM, Burtcel B, Kawabata H, Hodder S. (2002). "Young HIV-infected adults are at greater risk for medication nonadherence". MedGenMed. 4 (3): 21. PMID 12466764.
- ^ Nieuwkerk P, Sprangers M, Burger D, Hoetelmans RM, Hugen PW, Danner SA, van Der Ende ME, Schneider MM, Schrey G, Meenhorst PL, Sprenger HG, Kauffmann RH, Jambroes M, Chesney MA, de Wolf F, Lange JM and the ATHENA Project (2001). "Limited Patient Adherence to Highly Active Antiretroviral Therapy for HIV-1 Infection in an Observational Cohort Study". Arch. Intern. Med. 161 (16): 1962–1968. PMID 11525698.
- ^ Kleeberger C, Phair J, Strathdee S, Detels R, Kingsley L, Jacobson LP (2001). "Determinants of Heterogeneous Adherence to HIV-Antiretroviral Therapies in the Multicenter AIDS Cohort Study". J. Acquir. Immune Defic. Syndr. 26 (1): 82–92. PMID 11176272.
- ^ Heath KV, Singer J, O'Shaughnessy MV, Montaner JS, Hogg RS (2002). "Intentional Nonadherence Due to Adverse Symptoms Associated With Antiretroviral Therapy". J. Acquir. Immune Defic. Syndr. 31 (2): 211–217. PMID 12394800.
- ^ Burgoyne RW, Tan DH (March 2008). "Prolongation and quality of life for HIV-infected adults treated with highly active antiretroviral therapy (HAART): a balancing act". J. Antimicrob. Chemother. 61 (3): 469–73. doi:. PMID 18174196.
- ^ Karlsson Hedestam GB, Fouchier RA, Phogat S, Burton DR, Sodroski J, Wyatt RT (February 2008). "The challenges of eliciting neutralizing antibodies to HIV-1 and to influenza virus". Nat. Rev. Microbiol. 6 (2): 143–55. doi:. PMID 18197170.
- ^ Laurence J (2006). "Hepatitis A and B virus immunization in HIV-infected persons". AIDS Reader 16 (1): 15–17. PMID 16433468.
- ^ Planque S, Nishiyama Y, Taguchi H, Salas M, Hanson C, Paul S (June 2008). "Catalytic antibodies to HIV: Physiological role and potential clinical utility". Autoimmun Rev 7 (6): 473–9. doi:. PMID 18558365. Retrieved on 2008-07-17.
- ^ a b Power R, Gore-Felton C, Vosvick M, Israelski DM, Spiegel D (June 2002). "HIV: effectiveness of complementary and alternative medicine". Prim. Care 29 (2): 361–78. PMID 12391716. Retrieved on 2008-04-28.
- ^ Nicholas PK, Kemppainen JK, Canaval GE, et al (February 2007). "Symptom management and self-care for peripheral neuropathy in HIV/AIDS". AIDS Care 19 (2): 179–89. doi:. PMID 17364396. Retrieved on 2008-04-28.
- ^ Liu JP, Manheimer E, Yang M (2005). "Herbal medicines for treating HIV infection and AIDS". Cochrane Database Syst Rev (3): CD003937. doi:. PMID 16034917. Retrieved on 2008-04-28.
- ^ a b Irlam JH, Visser ME, Rollins N, Siegfried N (2005). "Micronutrient supplementation in children and adults with HIV infection". Cochrane Database Syst Rev (4): CD003650. doi:. PMID 16235333.
- ^ Hurwitz BE, Klaus JR, Llabre MM, et al (January 2007). "Suppression of human immunodeficiency virus type 1 viral load with selenium supplementation: a randomized controlled trial". Arch. Intern. Med. 167 (2): 148–54. doi:. PMID 17242315. Retrieved on 2008-04-28.
- ^ Zwahlen M, Egger M. "Progression and mortality of untreated HIV-positive individuals living in resource-limited settings: update of literature review and evidence synthesis" (PDF). UNAIDS Obligation HQ/05/422204. Retrieved on 2008-03-19.
- ^ Knoll B, Lassmann B, Temesgen Z (2007). "Current status of HIV infection: a review for non-HIV-treating physicians". Int J Dermatol 46 (12): 1219–28. doi:. PMID 18173512.
- ^ a b Lawn SD (2004). "AIDS in Africa: the impact of coinfections on the pathogenesis of HIV-1 infection". J. Infect. Dis. 48 (1): 1–12. PMID 14667787.
- ^ Campbell GR, Watkins JD, Esquieu D, Pasquier E, Loret EP, Spector SA (2005). "The C terminus of HIV-1 Tat modulates the extent of CD178-mediated apoptosis of T cells". J. Biol. Chem. 280 (46): 38376–39382. PMID 16155003.
- ^ Senkaali D, Muwonge R, Morgan D, Yirrell D, Whitworth J, Kaleebu P (2005). "The relationship between HIV type 1 disease progression and V3 serotype in a rural Ugandan cohort". AIDS Res. Hum. Retroviruses. 20 (9): 932–937. PMID 15585080.
- ^ McNeil DG Jr (2007-11-20). "U.N. agency to say it overstated extent of H.I.V. cases by millions", New York Times. Retrieved on 2008-03-18.
- ^ Gottlieb MS (2006). "Pneumocystis pneumonia--Los Angeles. 1981". Am J Public Health 96 (6): 980–1; discussion 982–3. PMID 16714472.
- ^ a b Centers for Disease Control (CDC) (1982). "Opportunistic infections and Kaposi's sarcoma among Haitians in the United States". MMWR Morb Mortal Wkly Rep. 31 (26): 353–354; 360–361. PMID 6811853.
- ^ Altman LK (1982-05-11). "New homosexual disorder worries officials", The New York Times.
- ^ "Making Headway Under Hellacious Circumstances" (PDF). American Association for the Advancement of Science (2006-07-28). Retrieved on 2008-06-23.
- ^ Kher U (1982-07-27). "A Name for the Plague", Time. Retrieved on 2008-03-10.
- ^ Centers for Disease Control (CDC) (1982). "Update on acquired immune deficiency syndrome (AIDS)—United States.". MMWR Morb Mortal Wkly Rep. 31 (37): 507–508; 513–514. PMID 6815471.
- ^ Curtis T. "The origin of AIDS", Rolling Stone, pp. 54–59, 61, 106, 108. Retrieved on 2008-03-10.
- ^ Hooper E (1999). The River : A Journey to the Source of HIV and AIDS, 1st, Boston, MA: Little Brown & Co, 1–1070. ISBN 0-316-37261-7.
- ^ Worobey M, Santiago ML, Keele BF, et al (2004). "Origin of AIDS: contaminated polio vaccine theory refuted". Nature 428 (6985): 820. doi:. PMID 15103367.
- ^ Berry N, Jenkins A, Martin J, et al (2005). "Mitochondrial DNA and retroviral RNA analyses of archival oral polio vaccine (OPV CHAT) materials: evidence of macaque nuclear sequences confirms substrate identity". Vaccine 23: 1639–1648. doi:. PMID 15705467.
- ^ "Oral Polio Vaccine and HIV / AIDS: Questions and Answers". Centers for Disease Control and Prevention (2004-03-23). Retrieved on 2006-11-20.
- ^ Gilbert MT, Rambaut A, Wlasiuk G, Spira TJ, Pitchenik AE, Worobey M (2007). "The emergence of HIV/AIDS in the Americas and beyond". Proc. Natl. Acad. Sci. U.S.A. 104 (47): 18566–70. doi:. PMID 17978186.
- ^ (2006) "The impact of AIDS on people and societies", 2006 Report on the global AIDS epidemic (PDF), UNAIDS. Retrieved on 2006-06-14.
- ^ Ogden J, Nyblade L (2005). "Common at its core: HIV-related stigma across contexts" (PDF). International Center for Research on Women. Retrieved on 2007-02-15.
- ^ a b c Herek GM, Capitanio JP (1999). "AIDS Stigma and sexual prejudice" (PDF). American Behavioral Scientist 42 (7): 1130-1147. doi:. Retrieved on 2006-03-27.
- ^ Snyder M, Omoto AM, Crain AL (1999). "Punished for their good deeds: stigmatization for AIDS volunteers". American Behavioral Scientist 42 (7): 1175–1192. doi:.
- ^ Herek GM, Capitanio JP, Widaman KF (2002). "HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999" (PDF). Am J Public Health 92 (3): 371–7. PMID 11867313. Retrieved on 2008-03-10.
- ^ a b Greener R (2002). "AIDS and macroeconomic impact", in S, Forsyth (ed.): State of The Art: AIDS and Economics. IAEN, 49–55.
- ^ Over M. "The macroeconomic impact of AIDS in Sub-Saharan Africa, Population and Human Resources Department" (PDF). The World Bank. Retrieved on 2008-05-03.
- ^ Duesberg PH (1988). "HIV is not the cause of AIDS". Science 241 (4865): 514, 517. doi:. PMID 3399880.
- ^ Papadopulos-Eleopulos E, Turner VF, Papadimitriou J, et al (2004). "A critique of the Montagnier evidence for the HIV/AIDS hypothesis". Med Hypotheses 63 (4): 597–601. doi:. PMID 15325002.
- ^ For evidence of the scientific consensus that HIV is the cause of AIDS, see (for example):
- , (2000). "The Durban Declaration". Nature 406 (6791): 15–6. doi:. PMID 10894520. Retrieved on 2008-05-03.
- Cohen J (1994). "The Duesberg Phenomenon: A Berkeley virologist and his supporters continue to argue that HIV is not the cause of AIDS. A 3-month investigation by Science evaluates their claims." (PDF). Science 266 (5191): 1642–1649.
- "Focus on the HIV-AIDS Connection: Resource links". National Institute of Allergy and Infectious Diseases. Retrieved on 2006-09-07.
- O'Brien SJ, Goedert JJ (1996). "HIV causes AIDS: Koch's postulates fulfilled". Curr. Opin. Immunol. 8 (5): 613–8. PMID 8902385.
- Galéa P, Chermann JC (1998). "HIV as the cause of AIDS and associated diseases". Genetica 104 (2): 133–42. PMID 10220906.
- ^ Smith TC, Novella SP (2007). "HIV denial in the Internet era". PLoS Med. 4 (8): e256. doi:. PMID 17713982.
- ^ Watson J (2006). "Scientists, activists sue South Africa's AIDS 'denialists'". Nat. Med. 12 (1): 6. doi:. PMID 16397537.
- ^ Baleta A (2003). "S Africa's AIDS activists accuse government of murder". Lancet 361 (9363): 1105. doi:. PMID 12672319.
- ^ Cohen J (2000). "South Africa's new enemy". Science 288 (5474): 2168–70. doi:. PMID 10896606.
Further reading
- "2007 AIDS epidemic update" (pdf). UNAIDS. Retrieved on 2008-03-21.
- "UNAIDS Annual Report - Making the money work" (pdf). UNAIDS. Retrieved on 2008-03-21.
- "Financial Resources Required to Achieve, Universal Access to HIV Prevention, Treatment Care and Support" (pdf). UNAIDS. Retrieved on 2008-03-21.
- "Practical Guidelines for Intensifying HIV Prevention" (pdf). UNAIDS. Retrieved on 2008-03-21.
- "Antiretroviral Formulations" (pdf). US Department of Health and Human Services. Retrieved on 2008-03-21.
- "Approved Medications to Treat HIV Infection" (pdf). US Department of Health and Human Services. Retrieved on 2008-03-21.
- "The HIV Life Cycle" (pdf). US Department of Health and Human Services. Retrieved on 2008-03-21.


No comments:
Post a Comment